
In modern dentistry, surgical insertion of implants into the missing teeth area has become a routine treatment method, but as the number of implanted implants and patients with implanted implants increases, inflammatory problems are increasingly being identified, which have progressed largely without the patient noticing their existence themselves.
Whether inflammation develops and if it develops as quickly as possible depends on many factors, but the main periimplant condition, like the exciting factor for periodontal conditions, is the bacterial application. If a doctor who advises and says putting implants in 100% of cases will solve the missing tooth problem without any risk of developing inflammation around an implant or even loss of an implant fails to provide objective information.
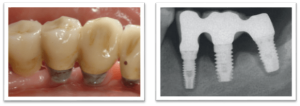
Inflammation, which develops around the implant, can only affect gum tissue, but, as inflammation progresses, without gum tissue, the bone already surrounding the implant. Therefore, there are two forms of periimplant disease: periimplant mucositis and periimplitis. In periimplant mucositis, inflammation is seen in soft tissue around the tooth implant, while periimplitis – free of inflammatory gum tissue – already shows bone breakdown, reduction in osseointegration, abnormal formation of periodontal pockets and possibly pus from them.
Usually, periimplitis prepares painlessly and symptoms can be felt relatively late in the patient when inflammation and bone loss around the implant have already developed strongly. Periimplitis itself “doesn’t hurt.” The implant area can only be sensitive when touching or cleaning the area, Diego. May have a bad taste in the mouth when pus is released. Local lymph nodes may increase in cases of severe inflammation.
Periimplitis affects a relatively small proportion of patients, but admittedly it is difficult to succumb to treatment.
First, the doctor conducts a thorough clinical and radiological examination for the exact diagnosis and preparation of the treatment plan before starting treatment, first by seriously motivating the patient to continue and regularly cooperate with oral health professionals to control the course of the disease, as well as by instructing on the necessity and technique of oral care.
For the most part, periimplant treatment is performed by surgery so that the implant surface can be efficiently treated and disinfected. If the possibility of regeneration is expected, biomaterials contributing to regeneration shall be used. In addition, antiseptics and, relatively often, antimicrobials are prescribed.
At times, the bone around the implant has been affected so badly that the implant needs to be removed and a serious rethink or put new one instead. Not all implants affected by periimplitis can be saved.